Table of Contents:
- What is Provider Data Management
- Why Health Systems and Hospitals Should Invest in Provider Data Management
- Reliable Provider Data is Needed to Power Multi-Channel Patient Access Initiatives
- Facilitating Optimal Patient-Provider Matching Accelerates Demand Conversion
- Managing Provider Networks Effectively Optimizes Capacity Utilization
- Centralizing Provider Data Enables Seamless Care Transitions that Boost Patient Retention
- Driving Operational Efficiencies and Growth by Maximizing Provider Data Utility Across the Organization
- Why Health Plans Should Invest in Provider Data Management
- Accurate and Robust Information Drives Member Attainment and Retention
- Enhancing Provider Data Closes Gaps in Care Access
- Addressing Data Inaccuracies Ensures Compliance and Reduces Risk of Penalties
- Building Impactful Partnerships with Providers Relies on Effective Provider Data Management
- Automating and Streamlining Provider Data Management Addresses Workforce Challenges
- Accurate Provider Data to Power the Future
Provider data lives in many places within health systems and health plans. There is information in spreadsheets, credentialing systems, EHRs, health plan directories, and many other locations. The maintenance of this information becomes cumbersome and very time-consuming, especially with frequent updates and many users.
As organizations look to drive digital transformation and take full advantage of new tools, centralized provider data management is critical. This solution resolves many of the data-oriented challenges healthcare organizations face today. Investing in a provider data management strategy offers organizations the ability to power enterprise-wide initiatives for patients, providers, and staff leveraging consistent data across access points—online provider directories, mobile apps, call centers, and more.
What is Provider Data Management?
Provider data is siloed. It often lives in multiple places across individual hospital departments, spreadsheets, and disparate databases. There are usually different stakeholders responsible for provider data accuracy—making it difficult to keep information up to date. When this happens, it often results in a poor consumer experience on an organization’s website. The information patients encounter such as location, or phone number might be wrong, leading to inaccurate provider directories and poor patient-provider matching.
Provider Data Management is the consolidation of all disparate data into a single source of truth. Once the source of truth is created, business rules can be put into place around the governance and upkeep of the provider data so that it can be properly maintained over time. Organizations may consider establishing role-based authorizations to enable administrators to control what information users can see and edit. It’s even possible to set up approval workflows to ensure proper checks and balances occur.
Why Health Systems and Hospitals Should Invest in Provider Data Management
An investment in a solid provider data management strategy is foundational. Not only does it power the consumer experience on an organization’s website and mobile app, but it can also be leveraged internally for various different use cases. Consider these 5 foundational reasons to invest in provider data management as you make a business case at your organization.
1. Reliable Provider Data is Needed to Power Multi-Channel Patient Access Initiatives
In order to guide patients to the right care, the information that is presented to consumers about your providers, locations, and services must be accurate and consistent across multiple access points. Without a provider data management system in place, information is often out-dated and inaccurate.
When a patient looks up a provider online and sees that they practice at a particular location, but then calls to make an appointment and learns that they are no longer at that location, it results in a frustrating patient experience. Consumers should have access to the same, accurate provider data regardless of where they are searching for care. Access should be consistent whether it’s on your website, via general internet searches, or a phone call into your organization. Providing this consistent experience to consumers across access points can go a long way in building trust.
2. Facilitating Optimal Patient-Provider Matching Accelerates Demand Conversion
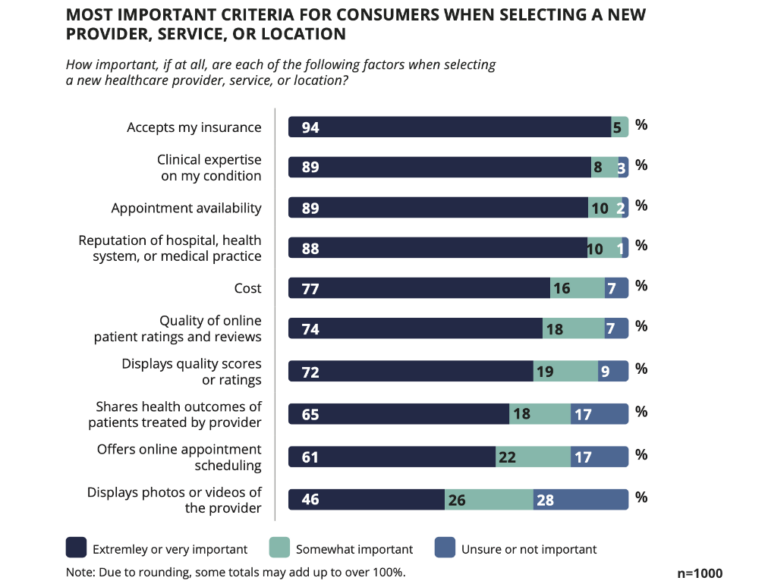
Organizations must ensure that the provider directories that house profiles are not only accurate, but complete with information that matters most to consumers when making a selection for their care. Attributes like insurance accepted (94%), clinical expertise (89%), and appointment availability (89%) all help convert patients looking to schedule appointments.
Many patients also like to have access to additional provider data. Some additions could be their professional statement, a video, whether they are LGBTQIA+ friendly, and more. This information can be extremely important as they are considering whether or not it will be a good patient-provider match. Given the option, many patients tend to choose providers based on shared traits.
When a provider data management strategy is in place, this information can all be managed in a single location. Provider data that may not have had a true “home” before such as marketing information like a biography, picture, or video, can all be maintained in a more streamlined manner.
Another key component of optimal patient-provider matching is ensuring that patients can easily search for a provider based on the specialty they need or symptoms they are experiencing. In many cases this includes lay synonyms such as “the sugars” for diabetes or “tennis elbow” for epicondylitis. Being able to layer on a robust clinical taxonomy that includes all of these different terms is a vital component of a well-rounded provider data management strategy.
3. Managing Provider Networks Effectively Optimizes Capacity Utilization
Given the current state of supply and demand issues in healthcare, it is more important than ever to have a clear view of your entire provider network. Consider leveraging a provider data management solution to help uncover and address gaps in provider types and services. Doing so can help you make strategic decisions about clinical recruiting to strengthen the integrity of your network.
When organizations have a more granular view into their network, they are able to adjust their access models to optimize capacity and improve appointment wait times. This might look something like, routing back to school physicals or flu shots to an APP such as a nurse practitioner or physician assistant instead of a primary care physician. This type of routing enables better management of capacity at an individual provider level, helping to ensure clinicians are not underutilized, overutilized, and/or misutilized.
4. Centralizing Provider Data Enables Seamless Care Transitions that Boost Patient Retention
Oftentimes when patients receive a referral from their physician or office staff, the information they are given is out of date, and the provider to whom they are referred may not be practicing any longer or may have left the organization. Provider data management can help solve this problem, as it can give all staff members accurate, reliable information at their fingertips.
This can be especially important for referring providers, who may go to an organization’s website to view physician profiles before determining an appropriate referral. It is vital that the information included on these profiles is accurate, so that providers can make the best choice for their patients.
Leveraging your provider data management system can help ensure a well-rounded view of an organization’s provider base. Having this accurate view will help empower clinical and administrative staff to guide patients during care transitions. Not only will they be able to connect patients to the most appropriate care, but they can do so in-network.
5. Driving Operational Efficiencies and Growth by Maximizing Provider Data Utility Across the Organization
At a time when resources are stretched thin, put your provider data management solution to work for you across the enterprise. This source of truth can be used throughout the organization in a myriad of ways, extending the utility of your provider data to internal assets such as call center operations, learning management systems, intranet pages, and more.
Maximizing provider data utility can help alleviate staffing challenges by eliminating the need for constant manual updates in multiple places, freeing staff up to focus on higher value tasks instead.
Having a centralized provider data management strategy is also extremely beneficial for organizations that may be in growth mode, whether it be organically or through M&A. Having a centralized, streamlined way to onboard the data for new physicians allows organizations to get them live on their website with accurate information much sooner then they would be able to otherwise.
Interested in learning more about provider data management for hospitals and health systems? Download our guide 5 Reasons to Prioritize Provider Data Management.
Why Health Plans Should Invest in Provider Data Management
Similar to hospitals and health systems, a provider data management strategy is essential for health plans to effectively power member experiences and internal processes. Here are five reasons why health plans should invest in provider data management.
1. Accurate and Robust Information Drives Member Attainment and Retention
When members search for healthcare providers online through their health plans, they expect a seamless and efficient process. However, they often encounter numerous obstacles such as outdated or incorrect information and a lack of comprehensive provider details like languages spoken, years in practice, and treatment philosophy. These deficiencies hinder their ability to find providers who align with their specific needs, leading to significant frustration among members.
A recent survey highlights that a vast majority of members desire more accurate and detailed information in provider profiles. Specifically, 62 percent of members are seeking more precise information, while 70 percent of Millennials and 64 percent of Gen Z members want more comprehensive details about providers. Enhancing the quality and accuracy of information provided by health plans can significantly improve member experiences, foster trust, lead to better healthcare outcomes, and increase member retention and acquisition. This improvement in service and information quality can also substantially boost a health plan’s financial performance, with potential gross margins ranging from $753 to $1,982 per attained enrollee.
2. Enhancing Provider Data Closes Gaps in Care Access
Inaccurate or incomplete provider data poses a significant barrier to accessing healthcare. Essential information like a provider’s gender, ethnicity, specialty, and experience is often missing from health plan directories, preventing members from finding a healthcare provider they trust and feel comfortable with. Discrepancies in provider data also result in “ghost networks,” where providers are listed as available but are not actually accessible. When members can’t find the information they need, they often delay or completely avoid seeking necessary care. One in three members have encountered inaccurate information in their health plan’s digital tools and 30 percent subsequently postponed or skipped care. This issue is compounded by the risk of members inadvertently using out-of-network providers, resulting in unexpected medical bills and increased administrative costs for health plans.
Another barrier to care is lack of online scheduling capabilities. Despite a strong desire among 80 percent of members to schedule appointments through their health plan’s website, over half have skipped care because this option was unavailable.
By integrating scheduling features and enhancing the accuracy of provider information, health plans can significantly improve member experiences, increase interactions with provider profiles, and thereby close care gaps.
3. Addressing Data Inaccuracies Ensures Compliance and Reduces Risk of Penalties
Recent regulatory mandates have been implemented to address the issue of poor data quality in health plans, emphasizing the importance of maintaining accurate provider data. For instance, the No Surprises Act requires health plans to verify their provider data quarterly and make necessary updates within two days. Non-compliance can lead to fines of up to $100 per day for each affected member. Additionally, the proposed REAL Health Providers Act aims to further tighten regulations by penalizing health plans for not correcting outdated information or removing providers who are no longer in-network, targeting the elimination of “ghost networks.”
While adhering to these regulations is crucial, the real challenge lies in how the updated information is presented to members. Many C-level executives in health plans recognize that enhancing the member experience is a significant challenge in meeting transparency mandates. For example, although health plans are required to publish machine-readable files with negotiated rates, this information often lacks the necessary context for members, featuring obscure billing codes that provide little value. Therefore, health plans need to go beyond mere compliance; they must ensure that the data is not only accurate but also accessible and understandable to members. This approach will make the information truly impactful, fulfilling more than just regulatory requirements and genuinely improving member satisfaction and trust.
4. Building Impactful Partnerships with Providers Relies on Effective Provider Data Management
Effective collaboration between providers and health plans is crucial for maintaining accurate and comprehensive provider directories. Providers rely on health plan portals to update their information, but they often face challenges such as inconsistent requirements and a cumbersome updating process. As a result, only 20 percent of providers feel confident that health plan directories accurately represent their facilities and staff. This disconnect highlights the need for improved systems and processes to ensure that provider information is both accurate and easy to update.
Almost all hospitals and health plans recognize the value in more detailed and robust information in provider directories. This is underscored by the fact that over a third of healthcare consumers are willing to switch providers for capabilities such as online appointment booking, which require accurate data. By investing in solutions that allow providers to directly and easily manage their profiles, health plans can streamline data maintenance, reduce labor costs, and ensure the accuracy and timeliness of the data. Establishing a centralized data repository can further enhance consistency across different channels, making updates more efficient and reliable.
5. Automating and Streamlining Provider Data Management Addresses Workforce Challenges
Managing provider data efficiently is crucial for health plans to avoid significant drains on resources. By addressing the root causes of inefficient data management and implementing systems that ensure data synchronization, health plans can prevent potential issues in downstream operations. A sophisticated provider data management platform can automate workflows and tasks, which not only saves time and costs, but also avoids the complications of developing such solutions in-house.
The accuracy of provider data across digital channels is essential, yet it’s important to recognize that many members still rely on direct interactions with providers or customer service to obtain healthcare information. Implementing a provider data management solution that offers real-time updates across all touchpoints ensures that everyone from call center agents to care navigators has access to the most current information.
Accurate Provider Data to Power the Future
As organizations look to embark on digital transformation, they will find that first investing in a solid provider data management strategy will help them be successful in the long run. Set your organization up for success with a digital experience that is powered by accurate, up-to-date information.